This emerging issue has given rise to a new metric in obesity care, namely, the quality of weight loss. The arrival of powerful GLP-1 receptor agonists such as semaglutide and tirzepatide has redefined what medicine can achieve in weight management. Double-digit weight loss once reserved for bariatric surgery is now possible with weekly injections. Yet behind these dramatic results lies a quieter concern: not all the lost weight is fat. Up to one-third of it may come from lean muscle mass, the tissue that drives metabolism, strength, and long-term energy balance.
This emerging issue has given rise to a new metric in obesity care, namely, the quality of weight loss. The question is shifting from “How much did you lose?” to “What did you lose?” In 2025, researchers, clinicians, and pharmaceutical developers are converging on this challenge from two directions. One is physiologic, optimizing protein intake and resistance training to preserve lean tissue. The other is pharmacologic, combining GLP-1s with new classes of drugs that block muscle-wasting pathways, such as anti-myostatin and activin inhibitors (notably trevogrumab and bimagrumab).
Together, these approaches mark the next evolution of metabolic medicine. As therapies become more potent, preserving muscle is emerging as both a clinical imperative and a market frontier, which is the key to making weight loss not only dramatic but also durable, functional, and healthy.
Why Now
The race to preserve muscle during weight loss has never been more urgent. While GLP-1 receptor agonists have revolutionized obesity care, recent clinical data have exposed a critical caveat: up to 30 40% of total weight lost on semaglutide or tirzepatide may come from lean mass rather than fat. That loss may translate into slower metabolism, reduced physical performance, and higher chances of regaining weight once treatment stops.
In 2025, the issue has moved from academic debate to headline status. The Endocrine Society’s ENDO 2025 conference featured multiple presentations focused on lean-mass preservation, including one from Dr. Jennifer Haines (Mass General) showing that modest resistance training and adequate protein intake can markedly blunt muscle loss in GLP-1 users.
At the same time, biotechnology firms are racing to commercialize pharmacologic answers. Drugs like bimagrumab (activin-receptor blocker) and trevogrumab (anti-myostatin/activin A antibody) have shown promise in preserving lean tissue when paired with GLP-1s, prompting analysts to project a >$30 billion market for “muscle-quality” therapeutics by 2035.
The convergence of clinical data, commercial momentum, and public attention makes 2025 the inflection point. The next question in obesity medicine is no longer simply how much weight patients lose, but what kind of weight they can afford to lose.
Why Muscle Preservation Matters
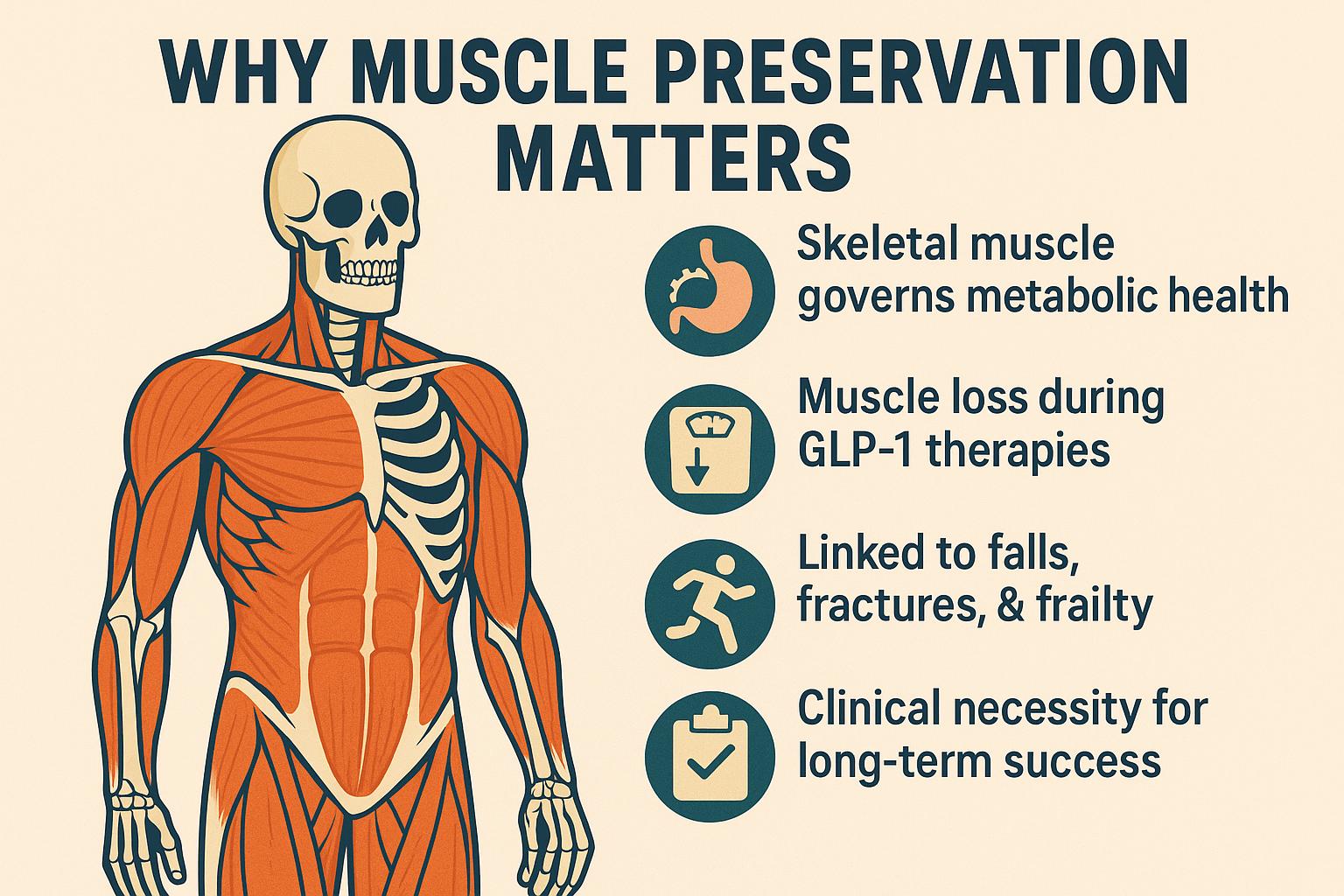
During GLP-1 therapy, studies show that as body weight falls, up to 40% of that loss can come from lean mass, particularly in older adults or those with low baseline protein intake. This can reduce basal metabolic rate by 5 10%, making it easier to regain fat once the medication is stopped. It can also impair insulin sensitivity and glucose tolerance, an ironic setback for patients taking GLP-1s for both obesity and diabetes prevention.
Clinically, this problem is especially pressing for sarcopenic obesity, where muscle loss coexists with high fat mass. Such patients risk losing the very tissue that protects their mobility, strength, and independence. In aging populations, even modest lean-mass reduction increases the likelihood of falls, fractures, and frailty.
Beyond physiology, there is a psychological and functional cost. Many patients describe fatigue, weakness, or slower recovery during physical activity while on GLP-1s. Those symptoms sometimes misattributed to calorie restriction alone. Emerging research suggests these may reflect underlying reductions in contractile tissue and mitochondrial capacity.
Preserving muscle, therefore, isn’t a cosmetic refinement; it’s a clinical necessity. As GLP-1 therapy becomes a lifelong management tool rather than a temporary fix, ensuring that weight loss targets fat rather than function will define the success or failure of this new generation of metabolic medicine.
Lifestyle Strategies
The most powerful tools for protecting muscle during GLP-1 induced weight loss remain the oldest ones, namely, adequate protein and resistance exercise. Both are strongly supported by data and immediately actionable in clinical practice.
Protein: More than Macronutrient Accounting
Weight loss on GLP-1s is largely driven by appetite suppression, which can reduce calorie and protein intake below the body’s needs for muscle maintenance. To counter this, experts now recommend a minimum of 1.2 1.5 g of protein per kilogram of body weight per day and up to 1.6 g/kg for older adults or those engaging in strength training. This intake supports muscle-protein synthesis, reduces nitrogen loss, and helps maintain satiety despite reduced overall calories.
The key, clinicians note, is distribution: roughly 25 30 g of high-quality protein at each meal provides the amino-acid threshold (especially leucine) needed to stimulate synthesis. Lean meats, fish, eggs, dairy, soy, and fortified shakes can help patients meet targets even when appetite is diminished.
Resistance Training: The Anabolic Signal
No nutrient can substitute for mechanical tension. Strength training two to three times per week, focusing on compound movements such as squats, rows, and presses, stimulates muscle growth and preserves neuromuscular integrity. In ENDO 2025 data presented by Haines et al., participants combining semaglutide with progressive resistance training retained ~85% of their lean mass, compared with ~65% in sedentary counterparts.
Short, structured workouts (30 40 minutes) can produce substantial benefits when combined with adequate protein and recovery. For patients with limited experience, body-weight routines or resistance bands provide an accessible entry point.
Bridging Lifestyle and Medicine
As new pharmacologic agents aim to spare muscle biochemically, lifestyle interventions remain the foundation of safe weight loss. GLP-1s may transform appetite and metabolism, but only strength training and protein ensure that what disappears on the scale is fat, not function. Clinicians increasingly view this triad (GLP-1 therapy + protein + resistance exercise) as the standard for sustainable, high-quality weight management.
Pharmacologic Advances
Much of this work focuses on the myostatin activin pathway, a key regulator that normally suppresses muscle growth. While lifestyle measures such as protein intake and resistance exercise remain the foundation of muscle preservation, biotechnology companies are now attempting to achieve the same goal pharmacologically. The rationale is straightforward: if GLP-1 drugs can reprogram metabolism to target fat loss, then additional agents might protect, or even rebuild, skeletal muscle at the same time.
Two leading candidates, bimagrumab and trevogrumab, have become central to this emerging field. In 2025, data from a mid-stage trial pairing bimagrumab with semaglutide drew wide attention after showing an average 22% total weight loss, of which an extraordinary 93% was fat mass. By contrast, semaglutide alone typically yields about 70% fat mass and 30% lean-mass reduction. These results, published in June 2025, suggested that selective inhibition of activin signaling could drastically improve the quality of weight loss, sparing metabolically valuable tissue.
A parallel program presented at the Endocrine Society’s ENDO 2025 meeting reported that trevogrumab combined with semaglutide preserved up to 80% of lean mass, compared with roughly 60% under GLP-1 monotherapy. Additional findings from Regeneron indicated improvements in muscle strength and reduced intramuscular fat infiltration among participants with type 2 diabetes.
The excitement has been tempered by setbacks: Eli Lilly halted development of a related candidate after safety and efficacy failed to meet expectations. Even so, analysts forecast a market exceeding $30 billion for therapies that optimize body composition rather than merely shrink weight.
The regulatory landscape is evolving alongside the science. The FDA has begun encouraging lean-mass outcomes in obesity-drug trials but remains cautious about possible off-target effects, such as fibrosis or altered insulin sensitivity. Though still investigational, these muscle-preserving combinations hint at a new horizon: pharmacologic weight-loss therapy that shapes metabolism instead of simply reducing it.
Integrative Approach
The ideal path forward is not an either or choice between exercise and drugs, but a synergistic strategy that merges behavioral and molecular interventions. The next frontier in obesity medicine is not simply losing weight, but recomposing the body, lowering fat while preserving, or even enhancing, muscle function.
In clinical practice, this means reframing the entire patient journey. Before initiating GLP-1 therapy, physicians are increasingly urged to obtain a baseline body-composition assessment using DXA or bioimpedance to quantify lean mass. Patients should begin a structured protein and resistance-training plan from the outset, not as an afterthought once weight loss slows. Progressive overload exercises two to three times per week combined with evenly distributed protein intake provide the necessary anabolic stimulus.
If future trials confirm the safety and efficacy of myostatin or activin inhibitors, these agents may become valuable adjuncts for individuals at high risk of muscle loss, such as older adults, those with sarcopenic obesity, or patients recovering from metabolic surgery. Such drugs could help maintain physical independence and metabolic resilience even during rapid GLP-1 induced fat reduction.
Implementing this integrative model will require cooperation among endocrinologists, dietitians, physiotherapists, and primary-care providers. Digital health tools, like wearable resistance trackers and nutrition apps, may help sustain adherence in real-world settings. Yet the philosophical shift is just as important, as weight management must evolve from a scale-centered paradigm to one that values function, composition, and quality of life.
As clinicians often summarize it: “The goal isn’t to weigh less, but to live better in the body you keep.” GLP-1s can open the metabolic door, but nutrition and strength training decide what walks through it.
Challenges & Future Outlook
Despite remarkable progress, the quest to improve the quality of weight loss faces scientific, clinical, and ethical hurdles. The most immediate challenge is data maturity: most trials of anti-myostatin or activin inhibitors remain small and short. While preliminary results suggest impressive preservation of lean mass, the true test will be whether this translates into better functional outcomes, i.e., strength, mobility, endurance, and long-term metabolic stability. Regulators such as the FDA have signaled growing interest in these endpoints but have not yet formalized approval pathways.
Safety and specificity remain key uncertainties. The myostatin/activin pathway influences multiple tissues, and sustained inhibition may carry off-target effects such as fibrosis or altered glucose handling. Balancing muscle preservation with systemic safety will determine whether these agents move from niche studies to mainstream obesity care.
Access is another major obstacle. Even if the science succeeds, high prices could restrict availability to elite clinics, deepening inequality in an already expensive therapeutic area. Ensuring affordability—and integrating lifestyle counseling rather than replacing it—will be essential for equitable adoption.
Finally, measurement and mindset must evolve. Routine DXA scans, grip-strength tests, and muscle-function assessments may soon join BMI and body weight as standard metrics. The future of weight management will not hinge solely on how light the patient becomes but on how strong, metabolically flexible, and resilient they remain.
In that sense, 2025 marks a turning point, the dawn of obesity care that values composition over reduction, and function over numbers.
References
-
Endocrine Society. (2025, June 2). Resistance training helps preserve lean mass in adults using GLP-1 medications, ENDO 2025 study finds.
https://www.endocrine.org/news-and-advocacy/news-room/endo-annual-meeting/endo-2025-press-releases/haines-press-release -
Reuters. (2025, June 20). Muscle-preserving drugs could generate over $30 billion in sales by 2035—TD Cowen.
https://www.reuters.com/business/healthcare-pharmaceuticals/muscle-preserving-drugs-could-generate-over-30-billion-sales-by-2035-td-cowen-2025-06-20/ -
Reuters. (2025, June 2). Regeneron’s weight-loss drug helps preserve muscle mass, study shows.
https://www.reuters.com/business/healthcare-pharmaceuticals/regenerons-weight-loss-drug-helps-preserve-muscle-mass-study-2025-06-02/ -
Reuters. (2025, Sept 25). Eli Lilly halts trial of experimental weight-loss drug.
https://www.reuters.com/business/healthcare-pharmaceuticals/eli-lilly-halts-trial-experimental-weight-loss-drug-2025-09-25/ -
Stat News. (2025, June 23). Bimagrumab combination achieves major fat loss while preserving muscle in Wegovy-style trial.
https://www.statnews.com/2025/06/23/bimagrumab-eli-lilly-study-results-wegovy-lean-muscle-mass-fat-weight-loss/ -
Mass General Advances in Motion. (2025, June 6). Preserving lean body mass in patients taking GLP-1 for weight loss.
https://advances.massgeneral.org/endocrinology/article.aspx?id=1601





